Physical Examination
After discussing your symptoms and medical history, your doctor will examine your shoulder. Your doctor will move your shoulder carefully in all directions to see if movement is limited and if pain occurs with the motion. The range of motion when someone else moves your shoulder is called “passive range of motion.” Your doctor will compare this to the range of motion you display when you move your shoulder on your own (“active range of motion”). People with frozen shoulder have limited range of motion both actively and passively.
Imaging Tests
Other tests that may help your doctor rule out other causes of stiffness and pain include:
- X-rays. Dense structures, such as bone, show up clearly on x-rays. X-rays may show other problems in your shoulder, such as arthritis.
- Magnetic resonance imaging (MRI) and ultrasound. These studies can create better images of soft tissues. They are not required to diagnose frozen shoulder, however, they may help to identify other problems in your shoulder, such as a torn rotator cuff.
Frozen shoulder generally gets better over time, although it may take up to 3 years. The focus of treatment is to control pain and restore motion and strength through physical therapy.
Nonsurgical Treatment
Most people with frozen shoulder improve with relatively simple treatments to control pain and restore motion.
- Non-steroidal anti-inflammatory medicines. Drugs like aspirin and ibuprofen reduce pain and swelling.
- Steroid injections. Cortisone is a powerful anti-inflammatory medicine that is injected directly into your shoulder joint.
- Hydrodilatation. If your symptoms are not relieved by other nonsurgical methods, your doctor may recommend hydrodilatation. This procedure involves gently injecting a large volume of sterile fluid into the shoulder joint to expand and stretch the shoulder joint capsule. Hydrodilatation is conducted by a radiologist who uses imaging to guide the placement of fluid.
- Physical therapy. Specific exercises will help restore motion. These may be done under the supervision of a physical therapist or via a home program. Therapy includes stretching or range of motion exercises for the shoulder. Sometimes heat is used to help loosen the shoulder up before stretching. Below are examples of some of the exercises that might be recommended.
- External rotation — passive stretch. Stand in a doorway and bend your affected arm’s elbow to 90 degrees to reach the doorjamb. Keep your hand in place and rotate your body as shown in the illustration. Hold for 30 seconds. Relax and repeat.
Surgical Treatment
If your symptoms are not relieved by therapy and other conservative methods, you and your doctor may discuss surgery. It is important to talk with your doctor about your potential for recovery continuing with simple treatments, and the risks involved with surgery.
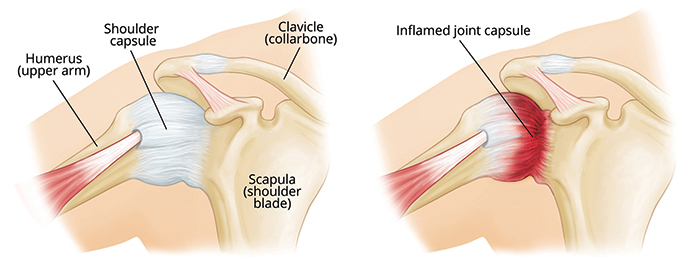
Surgery for frozen shoulder is typically offered during “Stage 2: Frozen.” The goal of surgery is to stretch and release the stiffened joint capsule. The most common methods include manipulation under anesthesia and shoulder arthroscopy.
- Manipulation under anesthesia. During this procedure, you are put to sleep. Your doctor will force your shoulder to move which causes the capsule and scar tissue to stretch or tear. This releases the tightening and increases range of motion.
- Shoulder arthroscopy. In this procedure, your doctor will cut through tight portions of the joint capsule. This is done using pencil-sized instruments inserted through small incisions around your shoulder.
In many cases, manipulation and arthroscopy are used in combination to obtain maximum results. Most patients have good outcomes with these procedures.
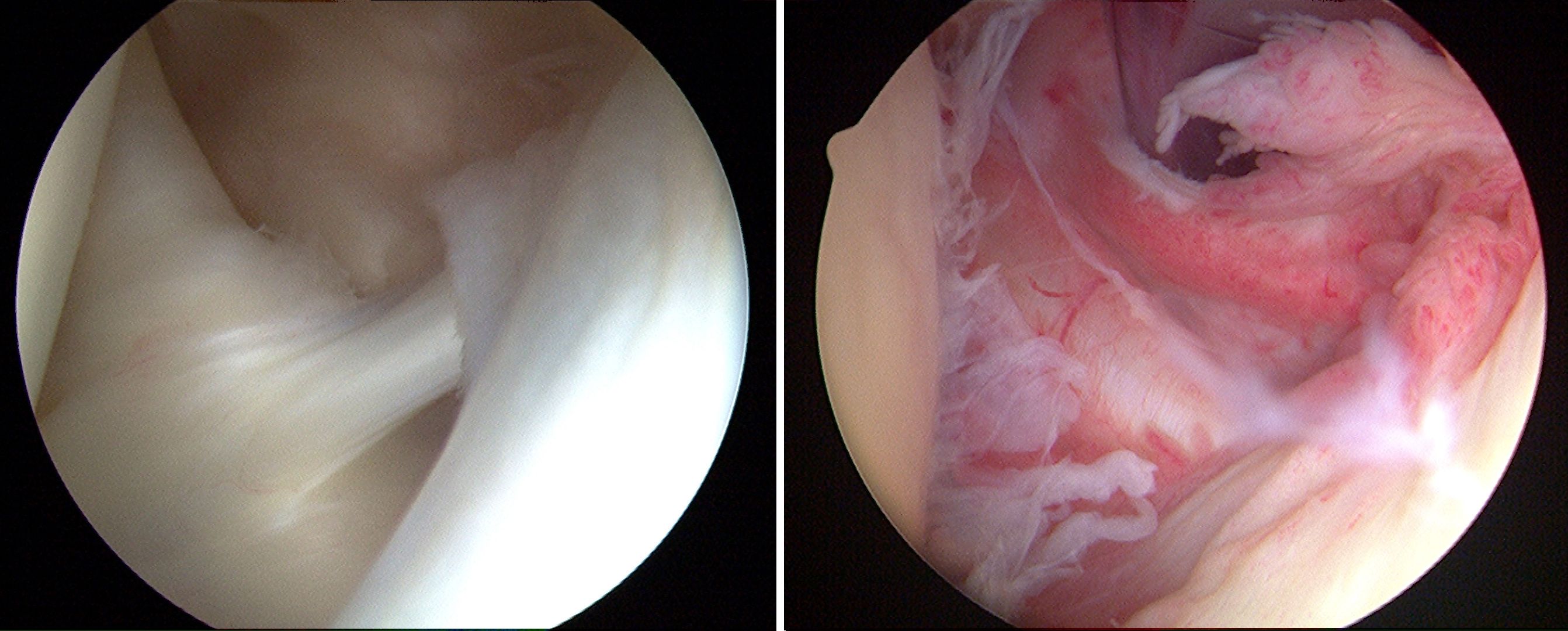
These photos taken through an arthroscope show a normal shoulder joint lining (left) and an inflamed joint lining affected by frozen shoulder.
Recovery. After surgery, physical therapy is necessary to maintain the motion that was achieved with surgery. Recovery times vary, from 6 weeks to 3 months. Although it is a slow process, your commitment to therapy is the most important factor in returning to all the activities you enjoy.
Long-term outcomes after surgery are generally good, with most patients having reduced or no pain and improved range of motion. In some cases, however, even after several years, the motion does not return completely and some degree of stiffness remains. Diabetic patients often have some degree of continued shoulder stiffness after surgery. Although uncommon, frozen shoulder can recur, especially if a contributing factor like diabetes is still present.



 / 159 Reviews
/ 159 Reviews